Treated conditions
Home » Areas of expertise » Arteriovenous malformations
Treated conditions
Arteriovenous malformations
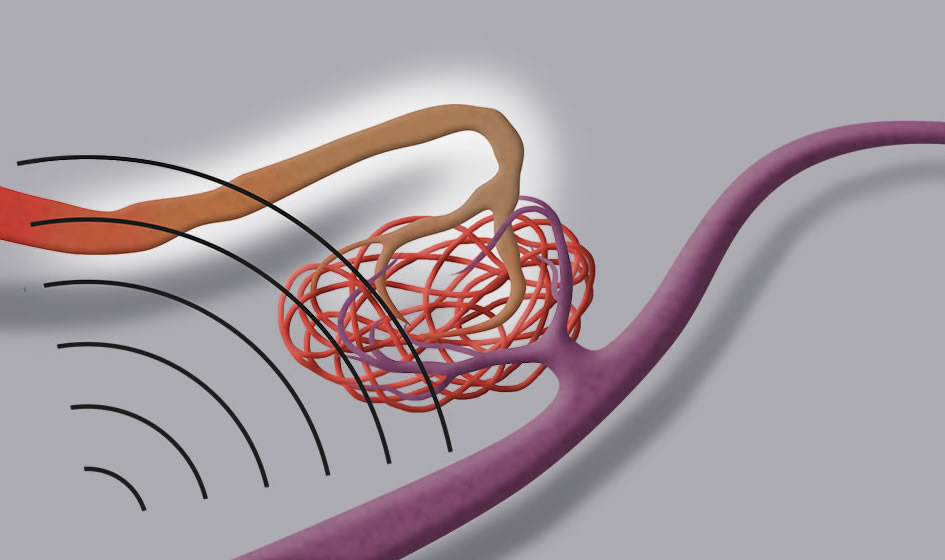
Arterio-venous malformations (also known with the acronym AVM) are a congenital anomaly of the cerebral vascular structures.
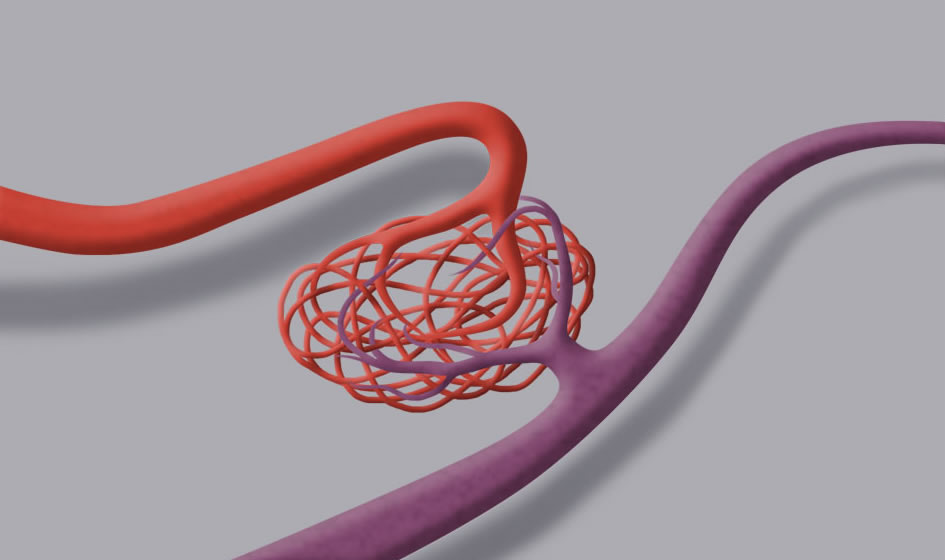
AVM implies that one or more large calibre arteries converge into a “tangle” of pathological vessels defined as nidus. From there, the blood coming from the arteries is conducted into one or more so-called arterialised venous discharges, since they transport the blood directly from the afferent arteries through the nidus itself but not, as is normally the case, through the tissues’ capillary bed, which physiologically reduces the pressure from arterial to venous.
A pressure overload on the damage of the nidus and of the venous discharges can lead to rupture of the AVM with consequent intracranial hemorrhage.
3% of the population carries arteriovenous malformations whose size can vary from just a few millimetres to larger diameters.
According to the Spetzler and Martin Grading Scale, AVMs are divided into 5 grades depending on the size of the nidus, its location in an eloquent or non-eloquent area, and on the presence of superficial or deep venous discharges.
This classification is used to assess the possibility as well as the most suitable type of treatment: grade 1 AVMs are the easiest to treat, while grade 5 are the most complex.
Symptoms
About 80% of all AVMs are asymptomatic, even if the anamnestic data shows that more than 50% of all patients report a long history of headache.
The clinical conditions vary depending on the location of the malformation, but generally they manifest themselves with seizures or intracranial hemorrhage.
Diagnosis
As for aneurysms, also the diagnosis of an AVM is often coincidental and can arise by means of a brain CT or MRI performed for other reasons.
The brain MRI allows for a correct assessment of the site and size of the malformation, especially if associated with an Angio-MRI or Angio-CT study.
However, contrary to cerebral aneurysms, a correct analysis of AVMs always requires a cerebral angiography, which, since it is a dynamic study, can reveal the precise architecture of the afferences, of the nidus, and of the venous discharges, as well as assess the speed with which the blood transits from the arterial to the venous compartment.
Angiography further makes it possible to reveal any aneurysms associated to the malformation or any arterio-venous fistulas inside or in the proximity of the nidus, which could increase the likelihood of future hemorrhages.
A functional brain MRI will make it possible to assess the relationship between the AVM and the so-called eloquent brain areas.
Treatment
The treatment of arterio-venous malformations is often multidisciplinary and includes microsurgery, endovascular treatment, and radiosurgery.
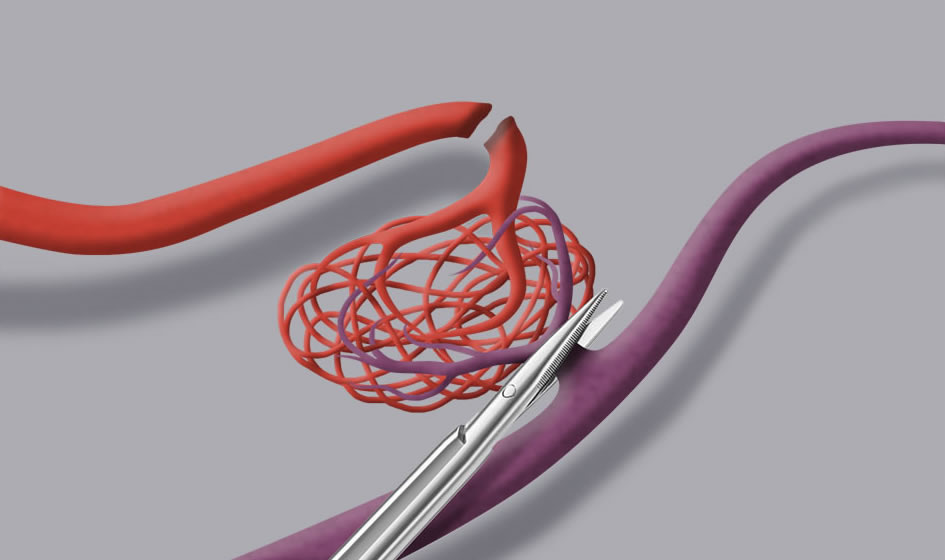
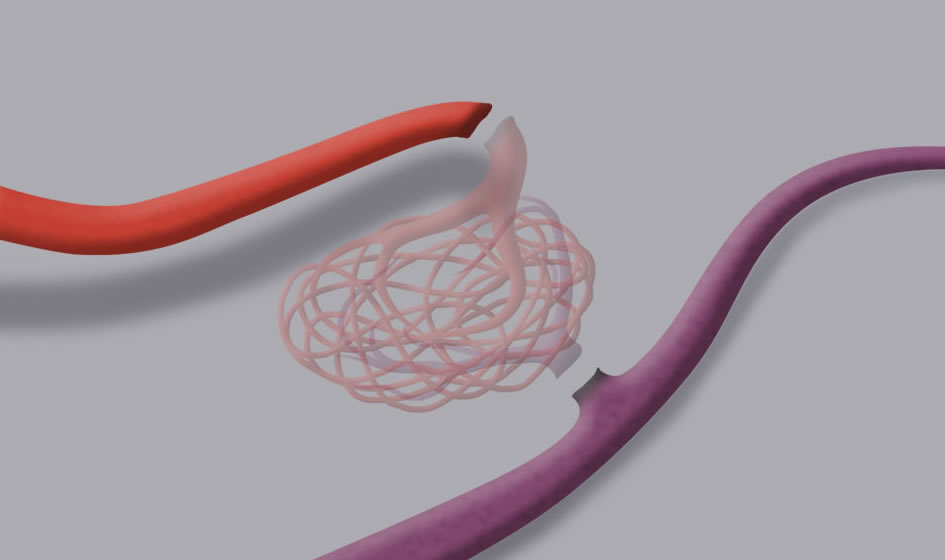
Microsurgical treatment consists in isolating the nidus by closing the feeders that provide it with blood (just like closing the taps). The progressive reduction of the blood flow will determine a slow “weakening” of the AVM. Once the nidus has been circumscribed, the venous discharges can be closed and the lesion can be removed in one piece. It should be stressed that inside the AVM there is no active brain tissue, but only a tangle of pathological vessels that can be removed.
Surgical treatment of AVMs should always be managed by neurosurgeons with a specific experience in this field, supported by a well-integrated team of anaesthesiologists and neurophysiologists in the operating room.
Surgery is performed by using the fundamental tools for a good outcome of the operation, such as an operating microscope with intraoperative fluorangiography, a neuronavigator, and intraoperative neurophysiological monitoring.
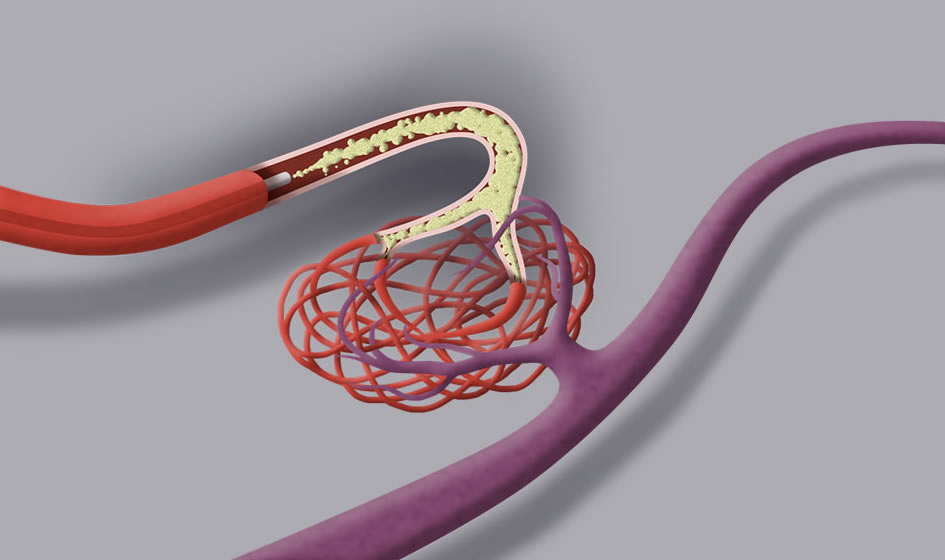
Endovascular treatment employs a microcatheter introduced in the femoral artery in order to reach the afferences of the malformation with the help of X-ray imaging. Once these have been reached, polymers are injected into the microcatheter in order to progressively reduce the blood flow inside the nidus.
Very often endovascular treatment is used with the aim of limiting the blood supply to the AVM in view of a surgical procedure (to make it easier and more safe), which will guarantee the total exclusion of the malformation.
In small AVMs, complete exclusion can be obtained only by means of the endovascular approach, without recurring to surgery.
Radiosurgical treatment consists in directing X-rays or gamma-rays on the AVM by means of collimators, with the aim of establishing a process of sclerosis in the walls of the vessels, which in time will cause the arterial afferences and the nidus to close.
Usually radiosurgical treatment is reserved for smaller AVMs (above 3 cm it is not very effective and there is a risk of relapse), located very deeply in the brain or in eloquent areas that have never bled, since this treatment can take up to 2 years to be effective. During this time span, the risk of bleeding is not excluded and remains unchanged.
To conclude, as in the case of cerebral aneurysms, there is no standard treatment for arterio-venous malformations, but they need to be assessed case by case in order to offer the best solution based on the location and the morphological characteristics of the AVM.